Colorectal Cancer
Editor-In-Chief: Dr. Heidi Kussmann, ND, FABNO
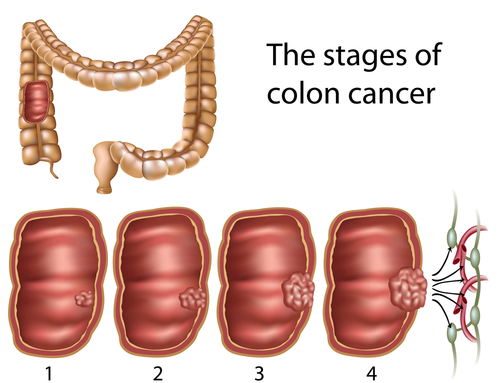
Colorectal cancer is a broad term describing cancer of the large intestine, sigmoid and rectum. It is further delineated into different types based upon the tissue involved. Most often the cancer that occurs in the colon above the anal verge is adenocarcinoma. Cancer at the anal verge is usually squamous cell or basal cell carcinomas. Carcinoid tumors are associated with the rectum and cecum. Colorectal cancer is rare below 40 years of age with the median age at diagnosis being 71.[1] Colorectal cancer is considered the third leading cause of cancer deaths in the US in men and women.
| Causes | Dietary Factors, Environmental Toxins, Infections, Smoking, Obesity |
|---|---|
| See Also | Women's Health, Oncology |
| Books | Books on Women's Health, Books on Oncology |
| Articles | Articles on Women's Health, Articles on Oncology (Cancer) |
| Article | Colorectal Cancer in Primary Care, NMJ, [2], 2012 April |
|---|
| Article | "Alcohol Consumption and Risk of Colorectal Cancer", NMJ, [3], 2011 December |
|---|
| Article | Dietary Glycemic Load and Colon Cancer , March 2013 Natural Medicine [4] |
|---|
Naturopathic Assessment
The diagnosis of colorectal cancer is typically made as a result of further investigation of concerning symptoms or as a positive result indicating abnormal findings from an annual fecal occult blood testing or a colonoscopy.
Causal Factors
In order to stimulate the innate ability of the body to heal the causes of disease must be identified and addressed. A detailed assessment is required to determine which factors are contributing to colorectal cancer.
Lifestyle
- Dietary imbalances, such as a diet low in fiber and high in fat is linked to colorectal cancer, according to the American Cancer Society.[2]
- A diet high in red and processed meat is associated with an increased risk of colorectal cancer.[3]
- Vitamin D deficiency is correlated to the development of colon cancer.[4]
- Obesity increases one's risk of developing colon cancer and decreases one's prognosis if they have colon cancer. [5]
Social
The social connections to colon cancer are difficult to determine as there are many social cultures with values and belief systems that influence one's decisions regarding health awareness. It is part of the epidemiological debate in defining the cause of many diseases, including cancer. In the realm of the social context, the following are known to increase the risk of colorectal cancer incidence:
- Socio-economic Status
- One study reported that since 1953 the increase of or change to higher socio-economic status and educational level in men correltate with the following types cancer incidence: colon, prostate, testis, kidney, and melanoma of the skin. In women the following cancers are related to higher social status and educational level: colon, breast and uterine.[6]
Environmental
- Infection with the Human Papilloma Virus (HPV) is a risk factor for the development of oral, anal, cervical and vulvar cancers. According to the Centers for Disease Control, HPV is a very common viral infection transmitted during sexual contact. A positive HPV test means that an HPV virus strain is present in the tested area of the body. Certain strains of HPV can lead to cancers of the cervix, mouth and throat, or anus. While testing for HPV on the cervix is common, some clinicians are also testing for HPV in the mouth and anus in high-risk patients. [7]
- Exposure to asbestos is associated with increased risk of colorectal cancer.
Medical Interventions
- Medical Treatments
- Radiation exposure can increase the risk of cancers, including colon cancer.
Genetics
- The majority of colorectal cancers are sporadic (not related to inherited genetics) rather than familial. However, it is more likely that an individual case of colorectal cancer has a familial link if the cancer developed prior to the age of 45 or if there are 2 first-degree relatives with colorectal cancer.[8]
- There is a 5-10% risk present with genetic colorectal diseases such as mutations in the APC gene to cause Familial Adenomatous Polyposis. 3-5% of all colorectal cancers being of the type called non-familial hereditary polyposis colon cancer or NHPCC. NHPCC occurs in younger people and can lead to the development of cancer in other areas of the body such as the endometrium, kidney and ureters, small intestine, and bile duct.
- More rare genetic disorders that lead to colon cancer include Turcot and Peutz-Jaghers Syndrome. Turcot Syndrome can also cause two forms of genetic mutations. Both result in brain cancer, either a glioblastoma or a medullaryblastoma. Peutz-Jaghers syndrome is caused by a genetic mutation of the STK1 gene. Mutations of the MUTYH gene causing MUTYH-associated polyposis. [9]
Physiology
- A change in bowel habits, especially if it correlated with increased frequency or looser stools, without a change in dietary habits may be significant.
Symptoms and Diagnostic Tests
The symptoms for colorectal cancer are nonspecific and include common systems that occur frequently in benign colon and digestive conditions such as such as anemia and abdominal pain.
- The presence of rectal bleeding or blood in the stool, both which are common benign symptoms, indicates the need to rule out colorectal cancer especially in individuals over the age 45.[10]
- Screening of colon cancer via annual fecal occult blood testing has proven successful in early detection which creates better clinical outcomes. [11] However, more reliable markers are needed especially if there are other remarkable signs or symptoms as this test has a high rate of false positives and false negatives.[12]
- Blood tests that are often requested included tumor markers such as CEA and CA 19-9, Liver function tests, CBC.
- Imaging Studies may include an abdominal ultrasound, contrast CT and/or MRI imaging may be used.
- Detection of colon cancer is usually confirmed histologically by biopsy after a colonscopy exam reveals significant findings.
- In those individuals with familial polyposis syndrome, or those where colorectal cancer is a high risk it is often beneficial to have regular colonoscopies to detect and remove any polyps which may be pre-cancerous.
Related Conditions
- According to the American Cancer Society, individuals with a history of ulcerative colitis, Crohn’s disease, or other inflammatory bowel diseases have an increased risk of colorectal cancer.
Naturopathic Treatment
The goal of naturopathic treatment is to support and work in tandem with the healing power of the body. A treatment strategy is the most effective when it addresses the underlying causal factors. The treatment for prostate cancer depends on the staging (progression) of the cancer, an individual's symptoms, vitality and other conditions.
It is always advisable to work with a naturopathic doctor before engaging in any treatment plan.
Prevention
Prevention involves addressing any of the causal factors before they cause cancer. Prevention in the form of lifestyle and dietary change is most effective if maintained over one's lifetime. Individuals with familial adenomatous polyposis, Crohns' Disease and Ulcerative Colitis are predisposed to inflammation at the cellular tissue level in the large intestine. The inflammation that occurs over the long term is related to poor dietary choices and unbalanced circadian regulation. As the inflammation continues over one's lifetime, the development of abnomal cells creates the histological changes seen in biopsy. One must actively strive to effect a sharp decline in total body inflammation in order to inhibit abnormal cellular proliferation [13] This includes regular daily aerobic exercise for at least 30 minutes, ingesting food that is high in soluble and insoluble fiber, high in antioxidants, and the process of decreasing and then eliminating foods which cause inflammation and GI distress symptoms. Additionally, research has indicated that an increase in ginger root in one's diet is also effective at decreasing the inflammation in the gut directly by inhibiting Cox-2. [14] [15]
Cancer Specific Treatments
Follow the general guidelines for cancer specific treatments. Additional treatments that are specific to colorectal cancer include:
- Dietary recommendations include increasing the intake of fiber and decreasing the consumption of fat.
| Article | Ginger May Reduce Colorectal Cancer Risk, NMJ, [5], 2012 June |
|---|
- Food Supplements include: melatonin, Vitamin D3, Modified Citrus Pectin, Plant Sterols, Quercetin, Resveratrol
- Herbs: Ginger (Zingiber officinale), Turmeric (Curcuma longa), green tea (Camellia sinensis), fermented wheat germ extract, Incense tree Boswellia (Boswellia serrata) Maitake & shiitake, ganoderma mushroom extracts.
Supportive Care
Follow the general guidelines for supportive care especially when conventional treatments such as surgery or radiation therapy are chosen.
- The complications of conventional treatment often include: neuropathy, diarrhea, constipation, hand foot syndrome, nausea, or bone marrow suppression. Less common but more serious complications include bowel obstruction, bowel perforation, or allergic reaction (anaphylaxis).
Naturopathic recommendations for the management of conventional oncology side effects depend on the side effect created. Understanding the chemotherapy mechanism of action and metabolism by the liver or kidneys will help to target and minimize potential side effects. Naturopathic recommendations are based from the modalities an ND is licensed to use and can range from acupuncture, high-dose vitamins and minerals to botanical medicines and homeopathy, and can additionally include IV therapy and nutritional support.
References
- ↑ Altekruse SF, Kosary CL, Krapcho M, et al. (2010) SEER Cancer Statistics Review, 1975-2007, National Cancer Institute. Bethesda, MD. [1]
- ↑ http://www.cancer.org/Cancer/ColonandRectumCancer/DetailedGuide/colorectal-cancer-risk-factors
- ↑ Chao A, Thun MJ, Connell CJ, et al. (2005) Meat consumption and risk of colorectal cancer. JAMA;293:172-182.
- ↑ Gorham ED, Garland CF, Garland FC, et al. Optimal vitamin D status for colorectal cancer prevention: a quantitative meta analysis. Am J Prev Med. 2007 Mar;32(3):210-6.
- ↑ Martinez ME, Giovannucci E, Spiegelman D, et al. Leisure-time physical activity, body size, and colon cancer in women. Nurses' Health Study Research Group. J Natl Cancer Inst. 1997;89:948-955.
- ↑ Rimpelä AH, Pukkala EI (1987) Cancers of affluence: Positive social class gradient and rising incidence trend in some cancer forms. Social Science & Medicine;24(7):601–606.
- ↑ http://www.cdc.gov/std/hpv/pap/default.htm#sec5
- ↑ Dunlop MG (2002) Guidance on large bowel surveillance for people with two first degree relatives with colorectal cancer or one first degree relative diagnosed with colorectal cancer under 45 years. Gut;51:17-20.
- ↑ http://www.cancer.org/Cancer/ColonandRectumCancer/DetailedGuide/colorectal-cancer-risk-factors
- ↑ du Toit J, Hamilton W, Barraclough K (2006) Risk in primary care of colorectal cancer from new onset rectal bleeding: 20 year prospective study. BMJ;333:69-70.
- ↑ Leo G. van Rossum, Anne F. van Rijn, Robert J. Laheij et al. Random Comparison of Guaiac and Immunochemical Fecal Occult Blood Tests for Colorectal Cancer in a Screening Population. Gastroenterology Volume 135, Issue 1, pp 82-90, July 2008.
- ↑ Graser A, Stieber P, Nagel D (2009) Comparison of CT colonography, colonoscopy, sigmoidoscopy and faecal occult blood tests for the detection of advanced adenoma in an average risk population. Gut;58:241-248. doi:10.1136/gut.2008.156448 Gutgut.bmj.com
- ↑ Backlund MG, Mann JR, Vijaykumar R et al. 15-Hydroxyprostaglandin Dehydrogenase Is Down-regulated in Colorectal Cancer. J. Biol. Chem. 2005 280: 3217-3223.
- ↑ Tjendraputra E, Tran VH, Liu-Brennan D, et al. (Jun 2001) Effect of Ginger Constituents and Synthetic Analogues on Cyclooxygenase-2 Enzyme in Intact Cells. Bioorganic Chemistry;29(3):156–163.
- ↑ van Breemen RB, Tao Y, Li W (Jan 2011) Cyclooxygenase-2 inhibitors in ginger (Zingiber officinale). Fitoterapia;82(1):38-43. Epub 2010 Sep 15.