Pancreatitis
| Causes | Dietary Factors, Alcohol, Genetics, Infections, Smoking |
|---|---|
| See Also | Endocrine Conditions, Diabetes, Chronic Alcoholism, Hyperlipidemia, Gallstones |
| Books | Books on Endocrine Diseases |
| Articles | Articles on Endocrine Conditions |
Pancreatitis is inflammation of the pancreas, which can range from mild to severe. The pancreas secretes insulin, glucagon and digestive enzymes which are normally activated in the gastrointestinal system. When the digestive enzymes become active within the pancreas, pancreatitis results. Pancreatitis may be experienced as an acute or chronic condition. Acute pancreatitis comes on suddenly and usually resolves within a few days with treatment, yet it can be life-threatening. Chronic pancreatitis needs to be managed closely and is often brought on by alcoholism or other underlying conditions.[1]
Naturopathic Assessment
Causal Factors
In order to stimulate the innate ability of the body to heal the causes of disease must be identified and addressed. Although alcoholism is the primary risk factor for pancreatitis, other factors need to considered.
Lifestyle
Environmental
- Certain infections (Ascaris lumbricoides, Cytomegalovirus, Coxsackie B virus, Mumps ).[3]
- Scorpion bites [4]
External
- Trauma
- Trauma or injury to the area of the pancreas can contribute to pancreatitis. [6]
Medical Interventions
- Prescription Medications
- Certain drugs may lead to the development of pancreatitis including:[3] azathioprine, 6-mercaptopurine, pentamidine, didanosine, sulfonamides, thiazides, aminosalicylates and valproic acid.
Genetics
- There seems to be a family predisposition.[7]
Diagnostic Testing
- The Blood tests that are commonly done include: amylase, lipase
- Imaging
- Abdominal X-ray, Abdominal ultrasound or CT scan
Related Symptoms and Conditions
Other conditions that increase the risk for pancreatitis include:
- Chronic alcoholism is one of the primary risk factors for chronic pancreatitis.[2]
- Diabetes increases ones risk of acute[8] and chronic pancreatitis.[9], [10]
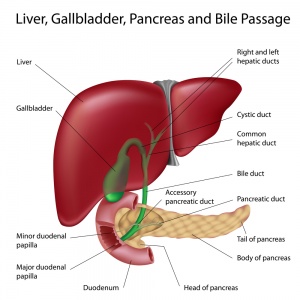
- Gallstones, especially when they obstruct the pancreatic duct, are often the trigger for acute pancreatitis.[11]
- High levels of lipid proteins in the blood .[1]
- Hypercalcemia or increased calcium in the blood is associated with increased risk.
Complications
The complication of pancreatitis, especially acute pancreatitis can affect several organ systems including the lungs, brain, heart, kidneys and bowel. Some of these complications include:[12]
- Dehydration
- Low blood pressure
- Shock
- Breathing problems
- Lung failure
- Kidney failure
- Pseudocyst formation
- Abscess formation
- Increased risk of infections
- Arrhythmia
- Multiple organ failure
- Ileus, or intestinal obstruction
Characteristics
There are four types of pancreatitis:
- Acute pancreatitis
- Chronic pancreatitis
- Pancreatic abscess
- Pancreatic pseudocyst
The symptoms associated with acute pancreatitis include:[13],[1]
- Abdominal pain, may radiate to the back
- Mild jaundice (yellowing of the skin)
- Nausea
- Vomiting
- Sweating
- Clammy skin
- Weakness
- Appetite loss
- Chills
- Fever
- Discoloration of the umbilical and flank region
- Fatty stools
Chronic pancreatitis may exhibit with some of the symptoms above, or it may be asymptomatic.
Naturopathic Treatment
The goal of naturopathic treatment is to support and work in tandem with the healing power of the body and to address the causal factors of disease with individual treatment strategies. If acute pancreatitis is suspected it is important to seek medical care right away due to the high risks that can be associated with this condition.
It is always advisable to work with a naturopathic doctor before engaging in any treatment plan.
Lifestyle
Lifestyle recommendations include:
- During an acute pancreatitis episode it is important to avoid eating or drinking anything by mouth. IV fluids can assist in ensuring that a person does not become dehydrated.
To prevent pancreatitis and in the treatment of chronic pancreatitis.
Naturopathic Therapies
The prescribing of naturopathic therapies requires the guidance of a naturopathic doctor as it depends on a number of factors including the causal factors, a person's age, prescription medications, other conditions and symptoms and overall health. It is always advisable to work with a naturopathic doctor prior to taking any natural therapies.
Naturopathic Therapies for pancreatitis include:
- Clinical Nutritional Supplementation includes
- Vitamins such as Vitamin A or beta-cartonene, Vitamin C, Vitamin D, Vitamin E, Vitamin K.[15] >, [16]
- Minerals such as selenium[16]
- Amino Acids such as methionine[16]
- Other supplements such as pancreatic enzymes[15],[17], Chlorophyll
- Herbs which may be helpful include Burdock root (Arctium lappa), Milk Thistle (Silybum marianum), Red Clover (Trifolium pratense), Echinacea (Echinacea angustifolia, Gentian Root (Gentiana lutea), Goldenseal (Hydrastis canadensis), Dandelion Root (Taraxacum officinale), Licorice Root (Glycyrrhiza glabra) and Olive leaf extract (Olea europaea).
- Homeopathic remedies such as Atropine, Kali iod, Mercurius, Iris, Iodum, Arsenicum iod, Phosphorus.[18]
References
- ↑ 1.0 1.1 1.2 Kumar R, Abbas A, DeLancey A, Malone E (2010) Robbins and Cotran Pathologic Basis of Disease. Eighth Edition. Saunders Elsevier.
- ↑ 2.0 2.1 Clemens DL, Mahan KJ (Mar 2010) Alcoholic pancreatitis: lessons from the liver. World J Gastroenterol;Vol16(11):1314-20. PMID: 20238397.
- ↑ 3.0 3.1 Forsmark CE. (2011) Goldman’s Cecil Medicine, 24th ed. [internet]. Saunders; Chapter 146 Pancreatitis. [cited 2012 Feb]. Available from: http://www.mdconsult.com.ezproxy.ndnet.ca/books/page.do?eid=4-u1.0-B978-1-4377-1604-7..00146-9&isbn=978-1-4377-1604-7&uniqId=316656842-3#4-u1.0-B978-1-4377-1604-7..00146-9--s0025
- ↑ Bartholomew C (Mar 1970) Acute Scorpion Pancreatitis in Trinidad. Br Med J;Vol1(5697):666-668. PMCID: PMC1700547.
- ↑ Alexandre M, Pandol SJ, Gorelick FS, Thrower EC (2011) The emerging role of smoking in the development of pancreatitis. Pancreatology;11(5):469-74. PMID: 21986098.
- ↑ Bradley EL 3rd. (1991) Chronic obstructive pancreatitis as a delayed complication of pancreatic trauma. HPB Surg;Vol5(1):49-59; discussion 59-60. PMID: 1777410.
- ↑ da Costa MZ, Guarita DR, Ono-Nita SK, Paranaguá-Vezozzo DC, Felga GE, Pedroso MR, de Souza MM, Nasser PD, Ferreira Cda S, Carrilho FJ (Jul 2011) Genetic risk for alcoholic chronic pancreatitis. Int J Environ Res Public Health;Vol8(7):2747-57. PMID: 21845156.
- ↑ Noel RA, Braun DK, Patterson RE, Bloomgren GL (May 2009) Increased risk of acute pancreatitis and biliary disease observed in patients with type 2 diabetes: a retrospective cohort study. Diabetes Care;32(5):834-8. PMID: 19208917.
- ↑ Braganza JM, Lee SH, McCloy RF, McMahon MJ (2011 Apr) Chronic pancreatitis Lancet; Vol377(9772):1184-97 PMID: 21397320.
- ↑ Malka D, Hammel P, Sauvanet A, Rufat P, O'Toole D, Bardet P, Belghiti J, Bernades P, Ruszniewski P, Lévy P (Nov 2000) Risk factors for diabetes mellitus in chronic pancreatitis. Gastroenterology;119(5):1324-32. PMID: 11054391.
- ↑ Whitcomb DC (May 2006) Acute Pancreatitis. N Engl J Med;Vol354:2142-2150.
- ↑ Waldthaler A, Schütte K, Malfertheiner P (2010) Causes and mechanisms in acute pancreatitis Dig Dis; Vol28(2):364-72 PMID: 20814214.
- ↑ Dains J, Baumann L, Schibel P (2007) Advanced Health Assessment and Clinical Diagnosis in Primary Care, ed 3. Mosby Elsevier
- ↑ Prousky Jonathan (2008) Principles and Practices of Naturopathic Clinical Nutrition, CCNM Press Inc.
- ↑ 15.0 15.1 El-Hashemy S (2011) Textbook of Naturopathic Family Medicine & Integrative Primary Care: Standards & Guidelines CCNM Press.
- ↑ 16.0 16.1 16.2 Kirk GR, White JS, McKie L, Stevenson M, Young I, Clements WD, Rowlands BJ (Apr 2006) Combined antioxidant therapy reduces pain and improves quality of life in chronic pancreatitis. J Gastrointest Surg;Vol10(4):499-503.
- ↑ Kirk GR, White JS, McKie L, Stevenson M, Young I, Clements WD, Rowlands BJ (Apr 2006) Combined antioxidant therapy reduces pain and improves quality of life in chronic pancreatitis. J Gastrointest Surg;10(4):499-503.
- ↑ Locke A (1998) The Family Guide to Homeopathy: The Safe Form of Medicine for the Future. Penguin.